Ever stood up from the couch and felt the room spin? Or struggled to pull off a ring that fit perfectly yesterday morning? They’re messages from your body about something fundamental going wrong with your hydration status.
Think of your internal water management system like the climate control in a luxury car, complex, precise, and absolutely essential for smooth operation. When things drift even slightly off course, you notice. The interesting part? Problems arise from both ends of the spectrum. Too little fluid causes issues. So does too much.
Learning to spot fluid imbalance symptoms early gives you a major advantage in preventing minor annoyances from becoming medical emergencies.
The Science Behind Fluid Balance
Water management in your body makes a city’s infrastructure look simple by comparison. This goes way beyond “drink eight glasses a day” territory, we’re talking about exact mineral concentrations and volume regulation across multiple biological compartments.
What Happens Inside Your Body
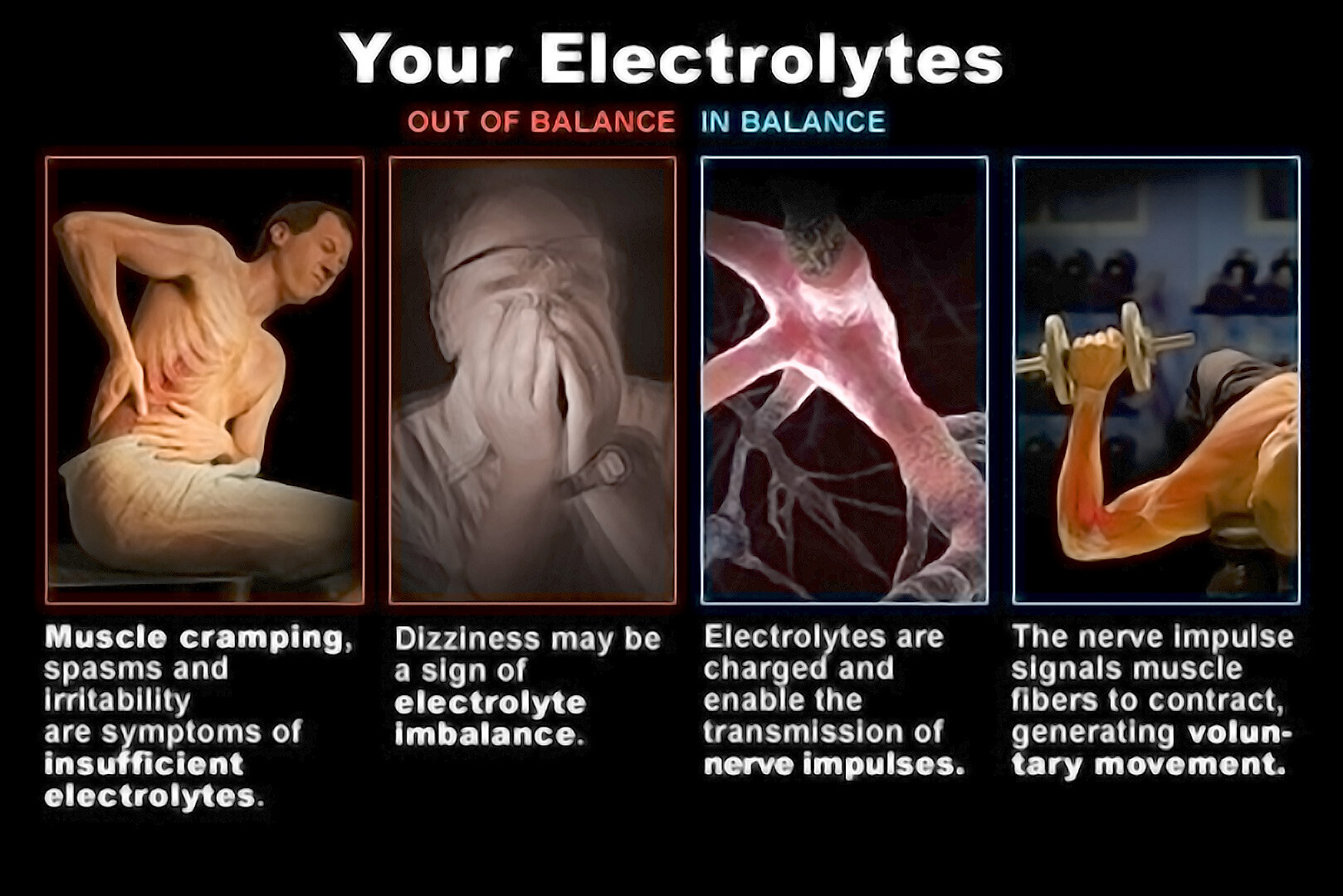
Water makes up roughly 60% of what you weigh. Electrolytes, sodium, potassium, chloride among others, function like border control agents. They determine where water can travel and where it stays put.
When these minerals drift outside their normal ranges, water tags along with them, triggering cascading effects that touch everything from cognitive clarity to cardiac rhythm. Meanwhile, your kidneys never sleep. They continuously recalibrate how much fluid leaves your body based on intake, sweat loss, respiration, and numerous other daily processes.
Why Balance Matters
Fluid disruptions create consequences extending far beyond personal discomfort. The healthcare system feels the impact too. Scientific investigations reveal that fluid overload correlates with extended hospital stays and elevated costs.
When your fluids drop too low, your body shifts into protective mode, blood vessels tighten, your heart works harder, and your system tries to conserve every drop. This is where people often begin to wonder, can dehydration cause high blood pressure, because that tightening effect can briefly push your numbers higher as your body struggles to maintain circulation.
Grasping these internal mechanics is valuable, but identifying when your precision system malfunctions? That’s where practical knowledge becomes lifesaving.
Recognizing the Warning Signs
Your body basically shouts at you when fluid levels veer too far either direction. The trick is learning the language it’s speaking.
When Your Body Needs Water
The signs of dehydration and overhydration look completely different from each other. Dehydration tends to announce itself more obviously. Your mouth gets that parched, sticky sensation. Urine shifts toward darker yellow or even amber territory. Headaches arrive uninvited, bringing fatigue that makes ordinary activities feel like marathons. Push further into dehydration territory and dizziness strikes, particularly during position changes. Your pulse rate climbs noticeably higher than usual.
Here’s something most people miss: fluid loss creates surprising effects on blood circulation patterns. Reduced water means decreased blood volume. Your heart compensates by pumping harder while blood vessels constrict to maintain pressure. This brings up a question patients frequently ask their doctors:can dehydration cause high blood pressure? Absolutely it can. Dehydration activates compensatory responses that temporarily spike blood pressure as your system fights to preserve adequate circulation to critical organs.
Too Much of a Good Thing
Overhydration operates more stealthily than its counterpart. Nausea appears without obvious cause. Swelling shows up in hands, feet, or around ankle areas. Headaches persist stubbornly. Mental fog rolls in unexpectedly. Severe overhydration dilutes sodium concentrations in blood, creating a condition called hyponatremia. Left unaddressed, this progresses to confusion, muscle weakness, potentially even seizures.
Body System Signals
Various systems react uniquely to hydration problems. Muscles cramp without warning, especially mid-workout. Joints feel stiff or achy despite proper rest. Your digestive tract joins the conversation, dehydration frequently brings constipation, while excess fluid might trigger bloating and abdominal discomfort. Even skin texture changes, with elasticity and appearance shifting based on hydration status.
Recognizing symptoms gives you defensive capability, but understanding root causes? That’s how you prevent problems before they materialize.
Understanding the Triggers
The effects of fluid imbalance on the body originate from lifestyle patterns, environmental exposures, and medical conditions that throw your natural equilibrium into chaos.
Daily Habits That Affect Balance
High temperatures and vigorous workouts accelerate fluid loss through perspiration. A challenging training session or afternoon working outdoors in summer might cost you multiple liters. Climate control systems (heating and AC) quietly steal moisture from your body by creating arid indoor atmospheres. Your morning coffee and evening wine increase urinary output, potentially pushing you toward dehydration unless you’re consciously replacing those losses. Even travel affects hydration, airplane cabins contain remarkably little humidity.
Medical Factors
Specific health conditions complicate the balancing act. Diabetes increases bathroom trips, elevating dehydration vulnerability. Kidney disease hampers your body’s regulatory capabilities. Heart failure can trigger fluid accumulation, leading to dangerous retention. Certain pharmaceuticals, diuretics and antihypertensive medications particularly, deliberately alter fluid dynamics and demand vigilant monitoring. The research presents sobering statistics: mortality rates reached 11.7% among pediatric intensive care unit patients experiencing fluid overload (pubmed.ncbi.nlm.nih.gov/39278783). That underscores just how serious severe imbalances become.
Now that you understand causative factors accurately, let’s explore targeted approaches for safely restoring equilibrium.
Getting Back on Track
Addressing fluid imbalances demands awareness paired with consistent action. Good news? Most individuals can effectively manage hydration through straightforward monitoring and adjustment techniques.
Practical Monitoring Methods
Mastering how to recognize fluid imbalance begins with noticing basic indicators your body provides constantly. Monitor urine color throughout your day, pale yellow suggests adequate hydration while dark amber screams for more fluids. Step on the scale at the same time each morning. Rapid gains of multiple pounds might flag fluid retention; losses suggest dehydration. Try the skin pinch test for immediate feedback. Pinch the skin on your hand’s back and release it. Immediate snapback typically indicates good hydration. Slow return suggests dehydration.
Smart Hydration Strategies
Maintaining proper body fluid balance doesn’t require obsessive glass-counting. Build consistent habits instead. Drink water alongside every meal. Keep a filled bottle within arm’s reach all day. During exercise or heat exposure, increase consumption before thirst appears, by the time you feel thirsty, you’re already behind.
Consider electrolyte-enhanced beverages during extended high-intensity activity exceeding an hour. Incorporate water-dense foods: cucumbers, watermelon, oranges. These contribute to hydration while delivering nutritional benefits. If retention becomes problematic, collaborate with your physician on appropriate sodium levels and potential medication modifications.
These fundamentals work well for most people, though specific populations face distinct hydration obstacles requiring customized solutions.
Taking Charge of Your Fluid Health
Your fluid regulation system operates continuously behind the curtain, but it requires your conscious participation to perform optimally. You’ve gained practical insights covering everything from early warning indicators like urine color shifts and energy fluctuations to understanding how dehydration influences blood pressure and additional vital functions.
Remember that optimal balance varies dramatically between individuals based on activity patterns, climate exposure, and underlying health conditions. Listen when your body communicates. Track fundamental indicators regularly. Seek professional medical guidance whenever symptoms persist or intensify. Small daily practices create the most significant long-term impact on keeping your internal hydration machinery running flawlessly for decades ahead.
Questions You Might Have
Does coffee really dehydrate you?
Coffee produces mild diuretic effects initially, but habitual consumption builds tolerance. Moderate coffee drinking actually contributes to daily fluid requirements. That said, exclusively relying on caffeinated drinks isn’t optimal since plain water remains your body’s preferred hydration source for peak performance.
How quickly can dehydration become dangerous?
Severity varies based on environmental conditions and individual characteristics. Under extreme heat or during intense physical exertion, dangerous dehydration can develop within mere hours. Elderly people and young children face amplified risks. Severe manifestations, confusion, racing heartbeat, urination cessation, demand immediate medical intervention.
Can drinking too much water actually harm you?
Definitely, though it happens less frequently than dehydration. Excessive water consumption dilutes blood sodium concentrations, producing hyponatremia. This typically occurs when people consume multiple liters within compressed timeframes, particularly during endurance competitions. Balance trumps maximization every time.